KERATOCONUS:
UPDATE
Prof M. R Jain FAMS
Medical DirectorM, R. J. Institute & Jain Eye Hospital, Jaipur
Keratoconus (from Greek: kerato- horn, cornea; and konos cone), is a degenerative disorder of the eye in which structural changes within the cornea cause it to thin and change to a more conical shape than its normal gradual spherical curve. In keratoconus, there can be substantial distortion of vision, with multiple images, streaking and sensitivity to light, all often reported by the patient. It is typically diagnosed in the patient's adolescent years and attains its most severe state in the twenties and thirties. If afflicting both eyes, the deterioration in vision can affect the patient's ability to drive a car or read normal print. In most cases, corrective spectacle lenses are effective enough to allow the patient to continue to drive legally and likewise function normally. But with the progress of the disease, the cone increases and the vision gets further deteriorated and the spectacle lenses are of not great help. The cone may take the shape of ‘nipple’ or may be ‘oval’ or may be ‘globus’ in appearance.
Symptoms and Signs
Keratoconus
can be difficult to detect, because it usually develops slowly. However, in
some cases, it may progress rapidly. As the cornea becomes more irregular in
shape, it causes progressive nearsightedness (myopia)
with high degree of irregular astigmatism, leading to distorted and blurred vision.
Glare and light sensitivity also may occur. Often, keratoconic patients
experience changes in their eyeglass
prescription every time they
visit their eye care
practitioner. In mild cases, the diagnosis may be delayed.
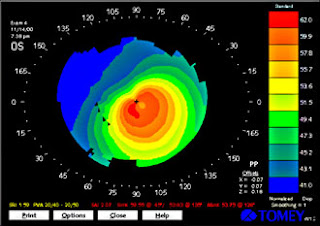
Placido’s
disc examination & Keratometry are easiest methods to diagnose keratoconus.
Orbscan gives detailed information about changes in the cornea.
What
Causes Keratoconus?
Recent research suggests weakening of the corneal tissue due to an
imbalance of enzymes within the cornea. This imbalance makes the cornea more
susceptible to oxidative damage from compounds called free radicals, causing it
to weaken and bulge forward. Genetic disposition leading to weakening of
cornea, explains familial incidence.
Keratoconus is also associated with
overexposure to ultraviolet rays from the sun, excessive eye rubbing, a
history of poorly fitted contact lenses and chronic eye irritation.
Rigid Gas Permeable Contact Lenses
When glasses fail to correct visual acuity, the best option is highly gas permeable semi soft contact lenses. The rigid lens material enables GP lenses to vault over the cornea, replacing its irregular shape. RGP lenses are initially more uncomfortable but in due course of time, patient gets well adapted. In moderate cases of keratoconus, contact lenses may provide 6/6 vision. FP 92 (Fluoroperm Siloxinate) manufactured by Paragon Vision Sciences can be worn during sleep without much discomfort. BostonXO & BostonO2 (B & L) with Dk Value of 100 & 141 respectively, are highly gas permeable. These lenses are made of Fluorosilicon Acrylate (FSA), having excellent wettability. There is special Keratoconus contact lens set which can help to fit a GP lens. In my practice I have found good acceptance by 90 percent of my early & moderately advanced keratoconus patients
Fig. Conventional RGP lens fitted in case of Keratoconus
In keratoconus, aspheric designs have proven to not only fit the varied corneal shapes, but also simplify the fitting process by eliminating some of the variables involved with lens design and fitting. These designs provide improved mid peripheral alignment as compared to spherical designs. Optical zone sizes are generally small but will usually accommodate the larger globus cones as well as oval or nipple type cones.
Piggybacking" contact lenses.
To provide better vision & make the fit more comfortable, Piggyback contact lenses are advocated in some cases of
keratoconus. This method involves placing a soft contact lens, such as one made of silicone hydrogel, over the eye and then fitting a GP lens over the soft lens. This approach increases wearer’s comfort because the soft lens acts like a cushioning pad under the rigid GP lens. I personally have not found these lenses satisfactory since the cornea is deprived of oxygen. These lenses are not much in use.
ClearKone hybrid contact lenses (SynergEyes Inc.,
These hybrid contact lenses combine a highly oxygen-permeable
rigid center with a soft peripheral "skirt." The ClearKone version was designed specifically for keratoconus and vaults above the
eye's cone shape for increased comfort. The hybrid contacts provide the crisp
optics of a GP lens and wearing comfort that rivals that of soft contact
lenses.
These lenses have to be
custom designed & hence they are extremely costly & as yet not
available in FIG. HYBRID CLEARKONE LENS
Rose K Lens
Rose-K lens introduced by New Zealand Optometrist, Dr. Paul Rose in 1989 & perfected it in year 2000. These lenses are latest innovation in the management of Keratoconus. Unlike traditional GP lenses, the complex geometry built into every Rose-K contact lens closely mimic the cone like shape of the cornea, for every stage of the condition. This enhances the fitting comfort of the contact lens as well provide better visual acuity.
The Rose K lens’s complex geometry has only become possible since computer controlled contact lens lathes were developed to cut sophisticated oxygen permeable polymers to the right shape. The practitioner has to maintain Rose-K trial set of 26 lenses to achieve successful fit.
The Rose
Paul Rose further improved the Rose-K lens which he labeled Rose
By nature, the keratoconic cornea is asymmetric, where the inferior quadrant is frequently significantly steeper than the superior portion, causing the GP lens to lift at 6 o clock position. Rose K lens incorporating ACT are designed to accommodate this asymmetry (good edge fit at 3, 9 and 12 o clock but lift at 6 o clock). The inferior quadrant of the lens is steeper than the superior quadrants, providing a more accurate fit at 6 o clock, there by enhancing the comfort & stability of the lens & vision. A toric periphery of Rose K2 lens (TP) further enhances the fit & improves vision. These lenses are manufactured by David Tomas, U K and are now available in
Apart from Keratoconus, Rose K lenses are also recommended for post keratoplasty astigmatism & post Lasik keratectasia.
Fig. Rose k lens fitted in keratoconus
Scleral and semi-scleral lenses (
These lenses are of only historical importance in the management of Keratoconus since the introduction of advanced management procedures including keratoplasty.
Intacs.(Addition Technology,
A recent surgical alternative to corneal transplant is the insertion of intrastromal corneal ring segments. A small incision is made in the periphery of the cornea and two thin arcs of polymethyl methacrylate are slid between the layers of the stroma on either side of the pupil before the incision is closed. The segments push out against the curvature of the cornea, flattening the peak of the cone and returning it to a more natural shape. The procedure, carried out on an outpatient basis under local anesthesia, offers the benefit of being reversible and even potentially exchangeable as it involves no removal of eye tissue. These inserts if required can be removed.
The principal intrastromal ring available is known by the trade name of Intacs. Internationally, Ferrara Rings are also available. Intacs are a patented technology and are placed outside the optical zone of 7.0 mm versus the smaller prismatic
FIG INTACS RING IN THE CORNEA
Collagen Cross Linking. (C3-R)
This non-invasive procedure strengthens corneal tissue to halt bulging of the eye's surface in keratoconus.
While various methods are under investigation, one brand name associated with the procedure is ‘corneal cross linking or C3-R (Boxer Wachler Vision,
In the
This simple treatment with or without INTACS might reduce significantly the need for corneal transplants among keratoconus patients. Corneal cross linking also is being investigated as a way to treat or prevent keratoconus-like complications following LASIK.
Fig. 10 diopters of corneal flattening after C3-R
Penetrating Keratoplasty
Between 10% and 25% of cases of keratoconus will progress to a point where vision correction is no longer possible, thinning of the cornea becomes excessive, or scarring as a result of contact lens wear causes problems of its own, and a corneal transplantation or penetrating keratoplasty becomes essential. Keratoconus is the most common ground for conducting a penetrating keratoplasty, generally accounting for around a quarter of such procedures with extremely rewarding results. Since most of keratoconus corneas have no vascular invasion & hence chances of stromal rejection is greatly reduced.
PK is a well-established technique. However, PK breaches the structural and immunologic integrity of the eye, thereby, exposing the eye to formidable challenge of endothelial rejection.
Deep Lamellar Keratoplasty (DLK)
Deep lamellar keratoplasty (DLK) is an effective alternative to penetrating keratoplasty (PK) with similar best-corrected visual acuity (BVCA) and refractive results, while reducing the risk of endothelial rejection in the surgical treatment of keratoconus.
In recent years, DLK techniques have improved so that a full-thickness corneal stroma and epithelial button may be placed into a host bed containing little or no stromal tissue on top of Descemet's membrane (DM).DLK is more technically challenging than PK but eliminates the possibility of endothelial rejection, has minimal effect on the endothelial cell count, and may reduce the risk of late endothelial failure.
The advancements in the last decade has given great relief to keratoconus patients. However, the management of Keratoconus continues to be a nightmare for the ophthalmic practiotioner. Proper understanding of the condition by the optometrist & an Ophthalmologist may significantly help the patient. In a myopic patient, constant increase in astigmatism & subnormal improvement of vision must alarm the eye care person.







This comment has been removed by the author.
ReplyDeleteNice blog
ReplyDeleteNow you can get the best and permanent treatment of Keratoconus from one of the leading Eye Specialists in Phagwara, Dr Harinder Mitra. Click on this link to make an appointment with Dr Harinder Mitra.
"I loved the blog content, please keep posting it. best keratoconus specialist "
ReplyDelete